Management guideline for rare irAEs (<1% incidence rate) and infusion-related reactions
International guideline (ASCO, ESMO and NCCN) recommendations for other irAEs1-3 ^
^ For detailed guidelines, please refer to original publication
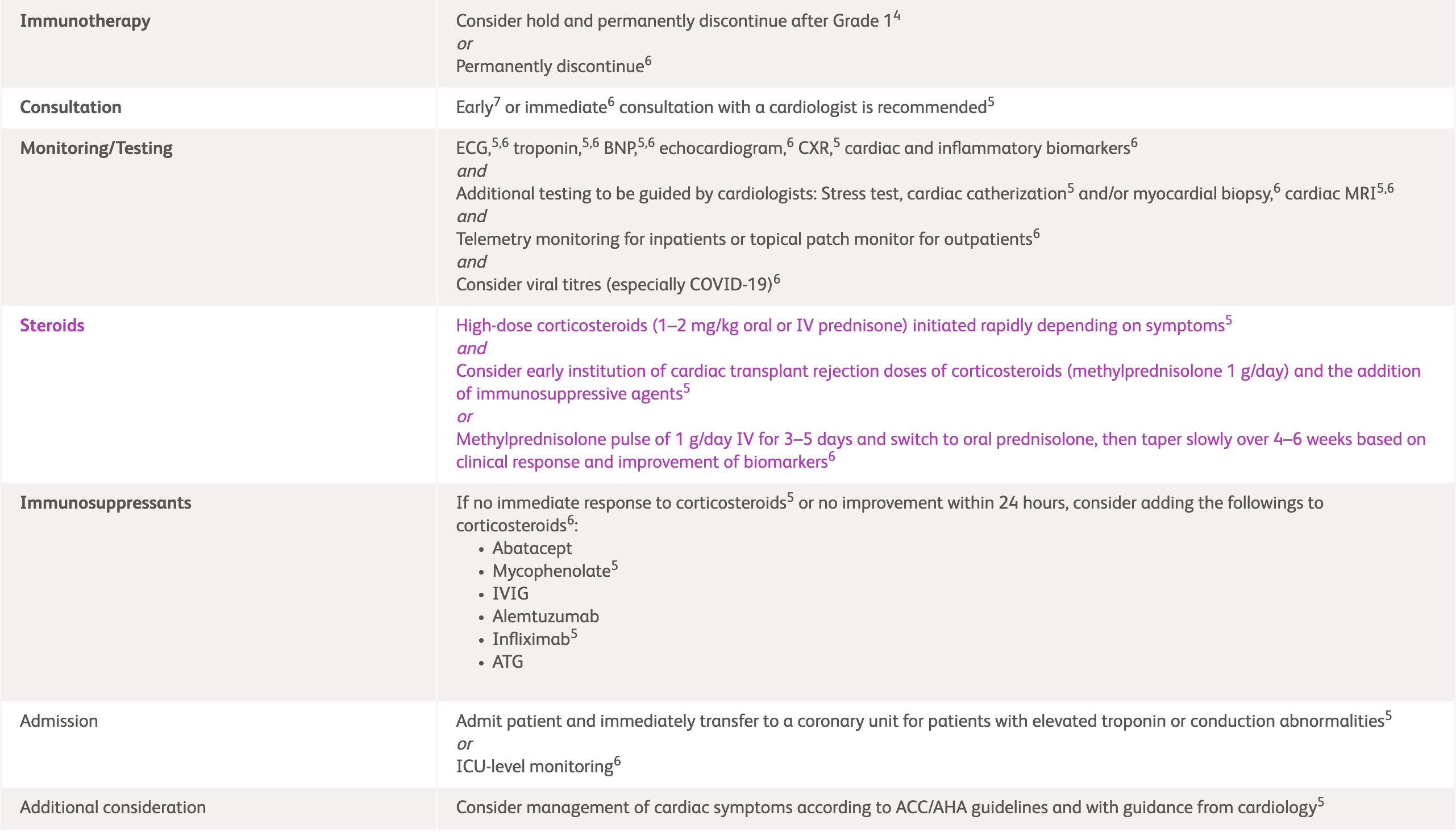
Suspected myocarditis, pericarditis, large vessel vasculitis
| Management | Grading/Assessment | |
|---|---|---|
| Myocarditis |
|
|
| Pericarditis/Pericardial effusion |
|
ECG, electrocardiogram; ICU, intensive care unit; irAEs, immune-related adverse events; IV, intravenous; IVIG, intravenous immunoglobulin; LV, left ventricle; NCCN, National Comprehensive Cancer Network.
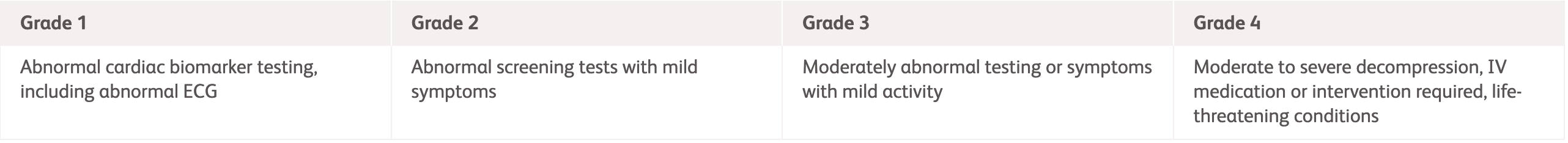
Myocarditis, pericarditis, arrhythmias, impaired ventricular function with heart failure, and vasculitis*
| Grading | Management | Assessment |
|---|---|---|
|
|
|
|
Grade 1:
Abnormal biomarker testing No symptoms No ECG abnormalities |
|
|
|
Grade 2:
Abnormal biomarker testing Mild symptoms New ECG abnormalities without conduction delay |
|
|
|
Grade 3:
Abnormal biomarker testing Moderate symptoms or new conduction delay |
||
|
Grade 4:
Moderate to severe decompensation IV medication or intervention required Life-threatening condition |
*Treatment recommendations are based on anecdotal evidence and the life threatening nature of cardiovascular complications. Holding checkpoint inhibitor therapy is recommended for all grades of complications. The appropriateness of rechallenging remains unknown. Note that infliximab has been associated with heart failure and is contraindicated at high doses (5 mg/kg) in patients with moderate-severe heart failure.
ASCO, American Society of Clinical Oncology; BNP, B-type natriuretic peptide; CPK, creatine phosphokinase; ECG, electrocardiogram; IV, intravenous; IVIG, intravenous immunoglobulin; MRI, magnetic resonance imaging.
Myocarditis
| Grading | Management and assessment (first 3 days) | |
|---|---|---|
| IR-myocarditis |
Management
|
Assessment
|
Management escalation |
Uncomplicated IR-myocarditis
|
|
|
Complicated IR-myocarditis
|
|
|
2L, second-line; 3L, third-line; ATG, antithymocyte globulin; CHB, complete heart block; ECG, electrocardiogram; ESMO, European Society for Medical Oncology; IR, immune-related; IV, intravenous; MFF, mycophenolate motefil; MDT, multidisciplinary team; MFF, mycophenolate motefil; MRI, magnetic resonance imaging.
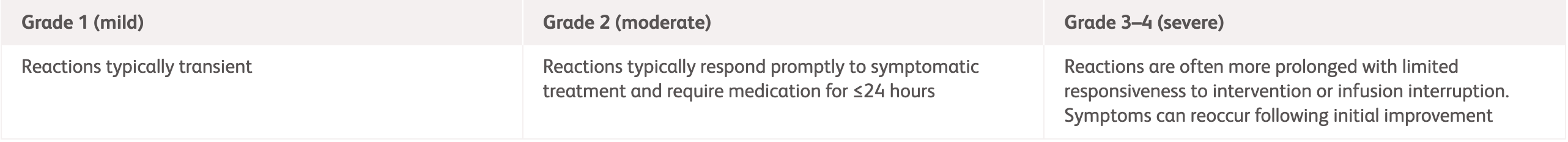
| Grading | NCCN2 | ASCO1 |
|---|---|---|
|
Grade 1
Mild transient reaction Infusion interruption not indicated Intervention not indicated |
|
|
|
Grade 2
Therapy or infusion interruption indicated but responds promptly to symptomatic treatment Prophylactic medication indicated for ≤24 hours |
|
|
|
Grade 3
Prolonged reaction (not rapidly responsive to symptomatic medication and/or brief interruption of infusion) Recurrence of symptoms following initial improvement Hospitalisation indicated for other clinical sequelae |
|
|
|
Grade 4
Life-threatening Urgent intervention indicated |
|
|
ASCO, American Society of Clinical Oncology; H2, histamine-2 receptor antagonists; IV, intravenous; ICU, intensive care unit; IV, intravenous; NCCN, National Comprehensive Cancer Network; NSAIDs, non-steroidal anti-inflammatory drugs.
References:
- Schneider BJ, et al. J Clin Oncol 2021;39:4073–4126. Available at: https://ascopubs.org/doi/full/10.1200/JCO.21.01440. Accessed April 2025.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Management of immunotherapy-Related Toxicities. Version 1.2025. Available at: https://www.nccn.org/professionals/physician_gls/pdf/immunotherapy.pdf. Accessed April 2025.
- Haanen J, et al. Ann Oncol 2022;33:1217–1238. Available at: https://www.annalsofoncology.org/article/S0923-7534(22)04187-4/fulltext. Accessed April 2025.
- OPDIVO® (nivolumab) Product Information, BMS Hong Kong.
- YERVOY® (ipilumab) Product Information, BMS Hong Kong.